Our Research
HER Salt Lake Posters
HER Salt Lake Presentations
HER Salt Lake Papers
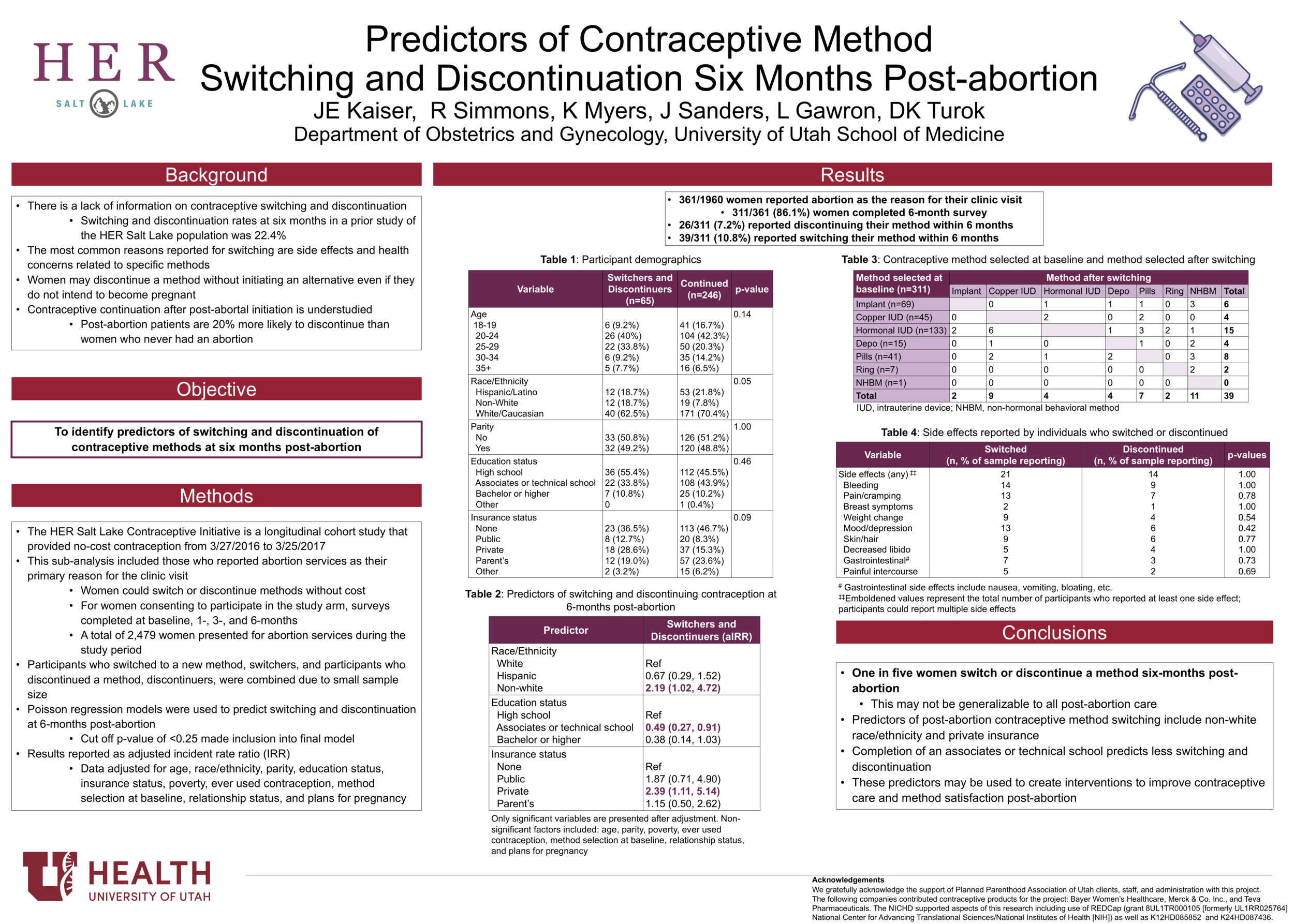
Predictors of Contraceptive Switching and Discontinuation within the First Six Months of Use Among HER Salt Lake Study Participants. Rebecca G. Simmons, Jessica N. Sanders, Claudia Geist, Lori Gawron, Kyl Myers, David K. Turok. American Journal of Obstetrics and Gynecology | April 2019
Read it here.
Background. Nearly half of women will switch or discontinue using their selected contraceptive method in the first year. Research on early switching or discontinuation provides important clinical and public health insights, though few studies have assessed associated factors, particularly among longitudinal cohorts.
Objectives. The current study explores attributes associated with early contraceptive method switching or discontinuation (<6 months of initiation) among participants enrolled in the intervention cohorts of the Highly Effective Reversible Contraceptive Initiative Salt Lake Contraceptive Initiative (Utah, United States).
Study Design. Highly Effective Reversible Contraceptive Initiative Salt Lake participants have access to no-cost contraception for 3 years. This includes both the initial selection and the ability to switch or to discontinue methods without cost. Methods available included the following: nonhormonal behavioral methods (male/female condoms, withdrawal, diaphragms, cervical caps, and fertility awareness); short-acting methods (pill, patch, ring, and injectable); and long-acting methods (intrauterine devices and contraceptive implants). Participants completed surveys at baseline and at 1, 3, and 6 months. We collected data on participant demographics, contraceptive continuation, switching, and discontinuation, as well as factors associated with these changes, including established measures of pregnancy intention and ambivalence and reasons for switching or discontinuing. We conducted descriptive statistics, univariable, and multivariable Poisson regression analyses to assess predictors of both discontinuation and switching. We also conducted χ2 analyses to compare reported reasons for stopping between switchers and discontinuers.
Results. At 6 months, 2,583 women (70.0%) reported continuation of their baseline method, 367 (10%) reported at least 1 period of discontinuation, 459 (12.4%) reported switching to a different method, and 279 (7.6%) did not provide 6-month follow-up. Factors associated with discontinuation included selection of a short-acting method (incidence rate ratio [IRR], 2.49; 95% confidence interval [CI], 1.97, 3.12), report of Hispanic ethnicity (IRR, 1.45; 95% CI, 1.12, 1.89) and nonwhite race (IRR, 1.48; 95% CI, 1.08, 2.02), and having any future pregnancy plans, even years out. Participants with some college education were less likely to report discontinuation (IRR, 0.73; 95% CI, 0.57, 0.94). Selecting a short-acting method at baseline was also associated with increased likelihood of method switching (IRR, 2.29, 95% CI, 1.87, 2.80), as was having 2 or more children (IRR, 1.37; 95% CI, 1.08, 1.74). Women were less likely to switch if they were on their parents’ insurance (IRR, 0.74; 95% CI, 0.56, 0.99). Among participants who switched methods, 36.9% switched to a long-acting reversible method, 31.7% switched to a short-acting hormonal method, and 31.1% switched to a nonhormonal behavioral method, such as condom use. Of participants providing a reason for stopping, 454 women (73.2%) reported side effects as 1 reason for switching or discontinuing their initial method.
Conclusions. Early contraceptive method switching and discontinuation are frequent outcomes of contraceptive use. These changes are common even with removal of contraceptive access barriers.
Beyond Intentions: The Relationship Between Feelings about Pregnancy and Contraceptive Choices. Claudia Geist, Jessica N. Sanders, Bethany Everett, Kyl Myers, Abigail Aiken, Patty Cason, & David K. Turok. Contraception. | August 2018
Read it here.
Objectives. To explore women's responses to PATH questions (Pregnancy Attitudes, Timing and How important is pregnancy prevention) about hypothetical pregnancies and associations with contraceptive method selection among individuals who present as new contraceptive clients and desire to prevent pregnancy for at least 1 year.
Study Design.The HER Salt Lake Contraceptive Initiative provided no-cost contraception to new contraceptive clients for 1 year at family planning health centers in Salt Lake County. Those who wanted to avoid pregnancy for at least 1 year and completed the enrollment survey are included in the current study. We used Poisson regression to explore the association between survey-adapted PATH questions and contraceptive method selection.
Results. Based on an analytic sample of 3121 individuals, we found pregnancy timing and happiness about hypothetical pregnancies to be associated with method selection. Clients who report plans to wait more than 5 years [prevalence rate (PR) 1.14; 95% confidence interval (CI) 1.05–1.24], those who never wanted to become pregnant (PR 1.16; 95% CI 1.07–1.26) or those who were uncertain (PR=1.19; 95% CI 1.09–1.30) were all more likely to select IUDs and implants than women who reported wanting to become pregnant within 5 years. Greater happiness was associated with lower chance of choosing an IUD or implant (PR 0.98; 95% CI 0.96–0.999). Expressed importance of pregnancy prevention was not significantly associated with any specific contraceptive choice.
Conclusions. Pregnancy intentions and happiness about a hypothetical pregnancy were independently associated with selection of IUDs and implants.
Implications. Pregnancy attitudes, plans and emotions inform clients' contraceptive needs and behaviors. Client-centered contraceptive care may benefit from a more nuanced PATH approach rather than relying on a single time-oriented question about pregnancy intention.
Contraceptive Method Use During the Community-Wide HER Salt Lake Contraceptive Initiative. Jessica N. Sanders, Kyl Myers, Lori Gawron, Rebecca G. Simmons, David K. Turok. American Journal of Public Health | February 2018
Read it here.
Objectives. To describe a community-wide contraception initiative and assess changes in methoduse when cost and access barriers are removed in an environment with client-centered counseling.
Methods. HER Salt Lake is a prospective cohort study occurring during three 6-month periods (September 2015 through March 2017) and nested in a quasiexperimental observational study. The sample was women aged 16 to 45 years receiving new contraceptive services at health centers in Salt Lake County, Utah. Following the control period, intervention 1 removed cost and ensured staffing and pharmacy stocking; intervention 2 introduced targeted electronic outreach. We used logistic regression and interrupted time series regression analyses to assess impact.
Results. New contraceptive services were provided to 4107 clients in the control period, 3995 in intervention 1, and 3407 in intervention 2. The odds of getting an intrauterine device or implant increased 1.6 times (95% confidence interval [CI] = 1.5, 1.6) during intervention 1 and 2.5 times (95% CI = 2.2, 2.8) during intervention 2, relative to the control period. Time series analysis demonstrated that participating health centers placed an additional 59 intrauterine devices and implants on average per month (95% CI = 13, 105) after intervention 1.
Conclusions. Removing client cost and increasing clinic capacity was associated with shifts in contraceptive method mix in an environment with client-centered counseling; targeted electronic outreach further augmented these results. (Am J Public Health. Published online ahead of print February 22, 2018: e1–e7. doi:10.2105/AJPH.2017.304299)
Acknowledgments
Support from the Society of Family Planning Research Fund, the William and Flora Hewlett Foundation, and an anonymous foundation. Contraceptive support from: Bayer Women’s Healthcare, Merck & Co. Inc., and Teva Pharmaceuticals. Use of REDCap provided by Eunice Kennedy Shriver National Institute of Child Health and Development grant (8UL1TR000105 (formerly UL1RR025764) NCATS/NIH). The Eunice Kennedy Shriver National Institute of Child Health & Human Development supports JNS via Award Number K12HD085852 and DKT via K24HD087436. We also want to thank the HER Salt Lake research team and all the participants.


![Dr. Rebecca Simmons | “Figuring out what I didn't like about all the previous [methods] led to knowing what I wanted better” | Oct 2019](https://images.squarespace-cdn.com/content/v1/576ac61f725e254d2ff438ef/1578616793561-FF5TNZDCE7R78A80KBPQ/Screen+Shot+2020-01-09+at+5.39.42+PM.png)